Stroke First Aid
A stroke is a medical emergency that can have severe repercussions.
If you suspect a stroke, time is of the essence, so do not delay in calling 000 for medical emergency services. First aid treatment for a stroke casualty aims to keep the victim as stable and comfortable as possible until emergency services arrive and take over.
Strokes can affect the way a person thinks, as well as their emotions.
Strokes vary in intensity and can affect different areas of the brain, causing problems with hearing, vision, speaking, memory, and muscle weakness.
If a person shows even one sign in the F.A.S.T. test below, call Triple Zero (000) straight away.
Prompt action can prevent further damage to the brain and help the casualty make a full recovery. Delay in getting treatment can result in death or major long-term disabilities.
While waiting for the ambulance, consult the following treatment plan:
A stroke occurs when the blood supply to a part of the brain is suddenly disrupted.
This can cause brain cells to die, as they rely on blood to receive life-sustaining oxygen and nutrients.
If a stroke victim does not receive prompt medical treatment, whole swathes of their brain can die, and they can sustain permanent brain damage and requisite physical, emotional, and intellectual complications.
Strokes can occur in three primary forms, each of which have their own individual causes:
Though they only last for a few minutes and do not generally cause long-term brain damage, TIAs should receive prompt medical treatment, as they indicate that the casualty could experience a full stroke within the next few days or weeks.
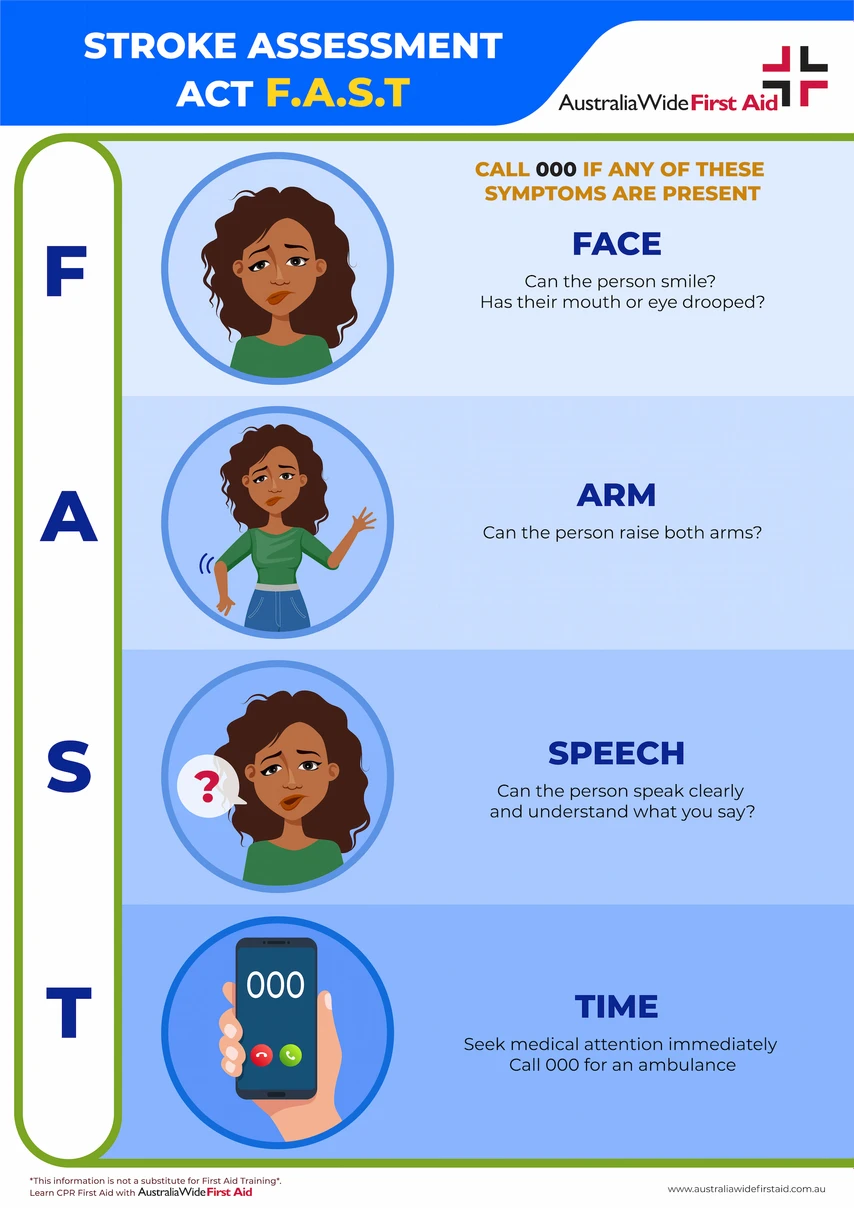
The Stroke Foundation recommends using the F.A.S.T test to remember the main symptoms of stroke.
As cited by the American Stroke Association, the acronym F.A.S.T represents:
The classic symptoms of a stroke begin suddenly and are pronounced. They include:
The symptoms of TIAs are indistinguishable from those of ischaemic or haemorrhagic strokes, though they tend to resolve themselves much more quickly.
As we mentioned earlier, even if a person experiences a TIA and only has difficulty speaking or moving for a brief period of time, they should still seek emergency care. That way, their risk factors can be proactively managed and their chances of a full ischaemic stroke reduced.
You should also call 000 even if someone fails the F.A.S.T test but does not experience any pain, as strokes do not hurt for many people.
Stroke symptoms will typically last more than 24 hours. Some stroke symptoms may or may not resolve, even with therapy.
TIA symptoms last only briefly, resolving in about 1 to 5 minutes. Less frequently, they can take up to 24 hours to resolve.
A stroke is often a frightening event that can leave its victim shaken and confused. Added to that are the long-term effects such as impaired or permanent loss of function. Often a stroke is a life-changing event that requires the person to re-learn basic functions.
Stroke experiences vary and the long-term effects they cause can likewise vary greatly depending on which side of the brain was affected. Prompt treatment and rehabilitation can aid in recovery and improve the chances of regaining bodily function.
The emotional impact of stroke also takes its toll. Speaking, with friends, family, a therapist, or a support group will also aid in the recovery process.
At the hospital, the stroke patient would have a CT scan, MRI, or other imaging test, to rule out other possibilities, such as a brain tumour or drug reaction.
For ischaemic stroke, medication would be given to break up clotting.
This medication — recombinant tissue plasminogen activator (r-tPA, also called alteplase or Activase) — needs to be given intravenously within 4.5 hours of when symptoms started.
Doctors can also use endovascular therapy to treat ischaemic strokes directly within the blocked blood vessel.
Newer imaging technology has extended the time window for these procedures. Perfusion imaging tests (done with CT or MRI) help determine whether endovascular therapy is likely to be beneficial.
For haemorrhagic stroke, emergency treatment focuses on controlling bleeding and reducing pressure in the brain caused by the excess fluid.Unfortunately once someone has experienced a stroke, they are at a higher risk for a secondary stroke. Secondary stroke can have even more devastating effects than the first and increases the chances of death.
The risk of experiencing secondary stroke is highest in the following few days after the initial stroke and remains increased especially during the first year and up to five years. Taking steps for preventing any future stroke is crucial to ones survival.
Disclaimer: This article is for informational purposes only. It does not constitute, replace, or qualify as any form of first aid training.
For more information about the risk factors and signs of stroke, check out the National Stroke Foundation and their annual awareness campaigns, including National Stroke Week. The resources listed below are also useful for managing a variety of out-of-hospital emergencies:

March 18, 2025
Checking for a response is critical before proceeding with any first aid assistance. Knowing if a casualty is conscious or not allows you to use the appropriate techniques. Using gentle but firm responsiveness techniques, such as the COWS method, mean you can check for a response while remaining respectful to the casualty.

February 25, 2025
When coming across someone who appears unconscious, injured, or in need of medical help, it’s instinctive to rush to their aid. Ensuring the scene is safe before assisting the person is not only a fundamental principle of first aid but also critical to preventing further harm.

March 8, 2024
Becoming a first aid trainer in Australia is a rewarding and impactful career choice that allows individuals to make a significant contribution to the community by imparting life-saving skills.